Our Reversals Procedure
Reversal by Our Gold Standard Technique
Introduction – it is natural to think that a reversal is a reversal and that all operations are roughly the same so it is OK to shop around for the cheapest. So this presentation is to explain why we use the MMMV procedure which takes on average 3 hours to perform using expensive materials and gives the world’s best reversal results.
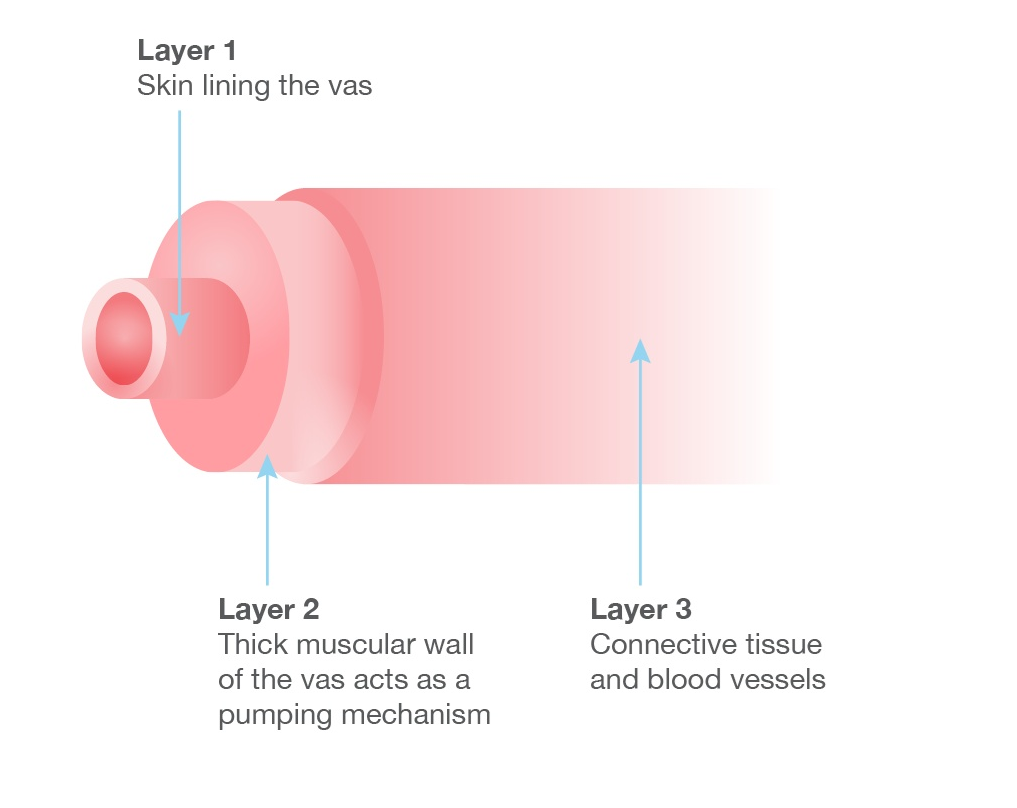
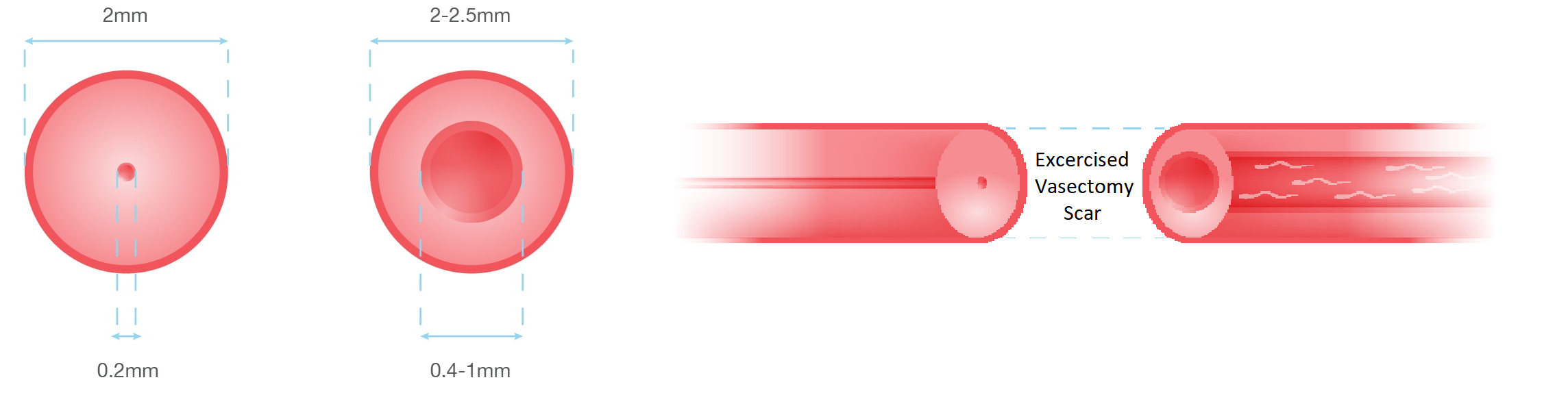
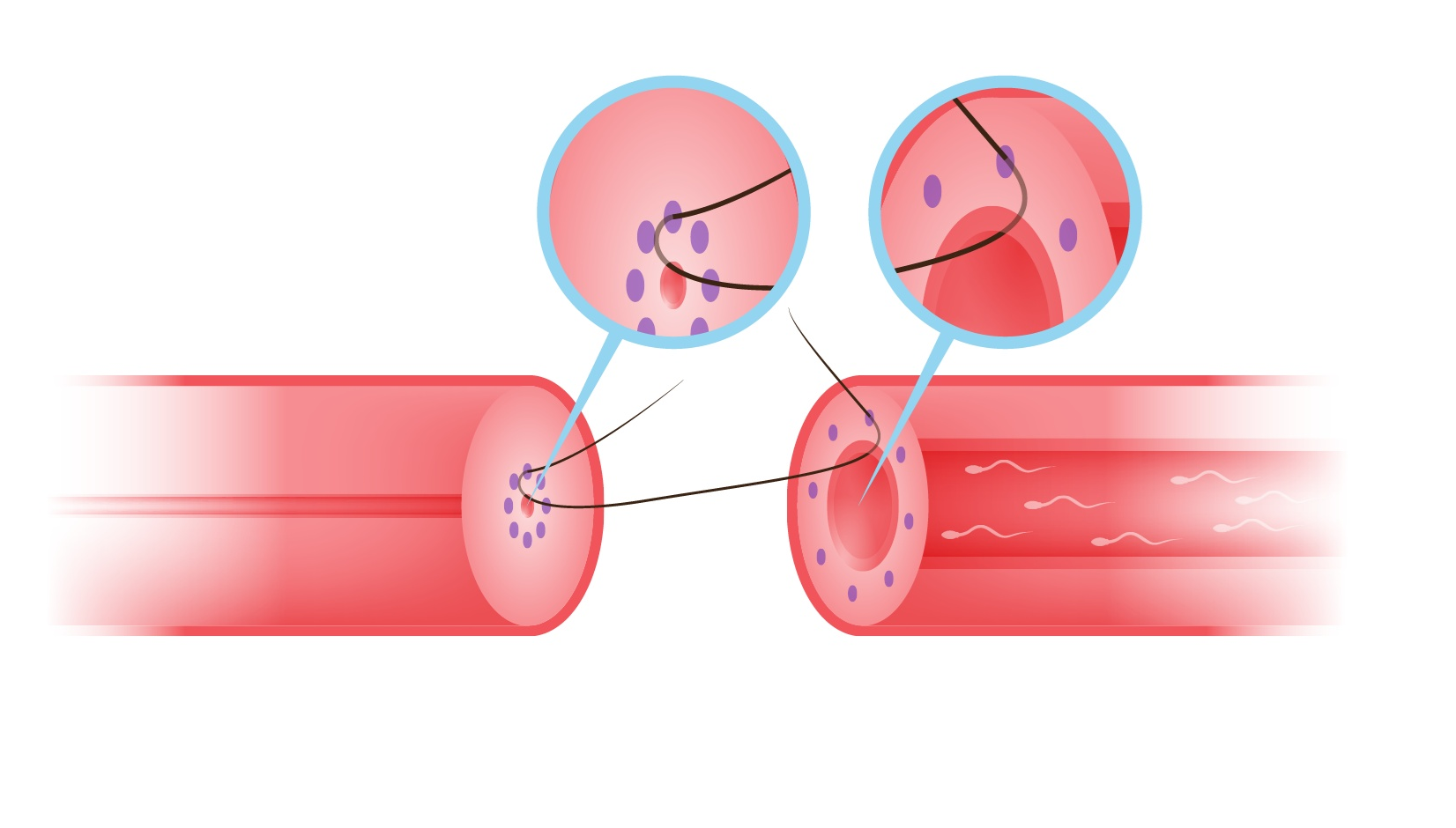
1. This is a diagram of the normal vas – a tiny (0.2 mm) sperm channel surrounded in a strong muscle coat and beyond that a layer of connective sinews and blood vessels. The overall diameter is around 2 mm.
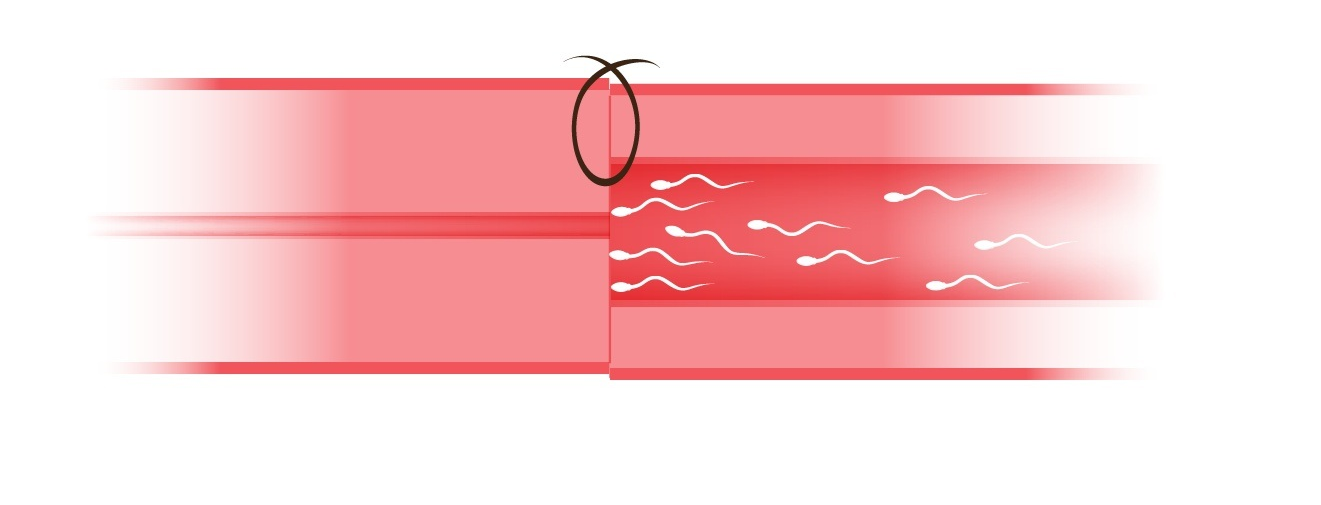
2. Following vasectomy, which simply blocks the vas, there is high pressure on the lower, testis side caused by the force of the sperms trying to escape. This causes the central sperm channel on the testis side to enlarge and dilate so that when we come to remove the vasectomy scar and rejoin the tube the two ends of vas look like this;
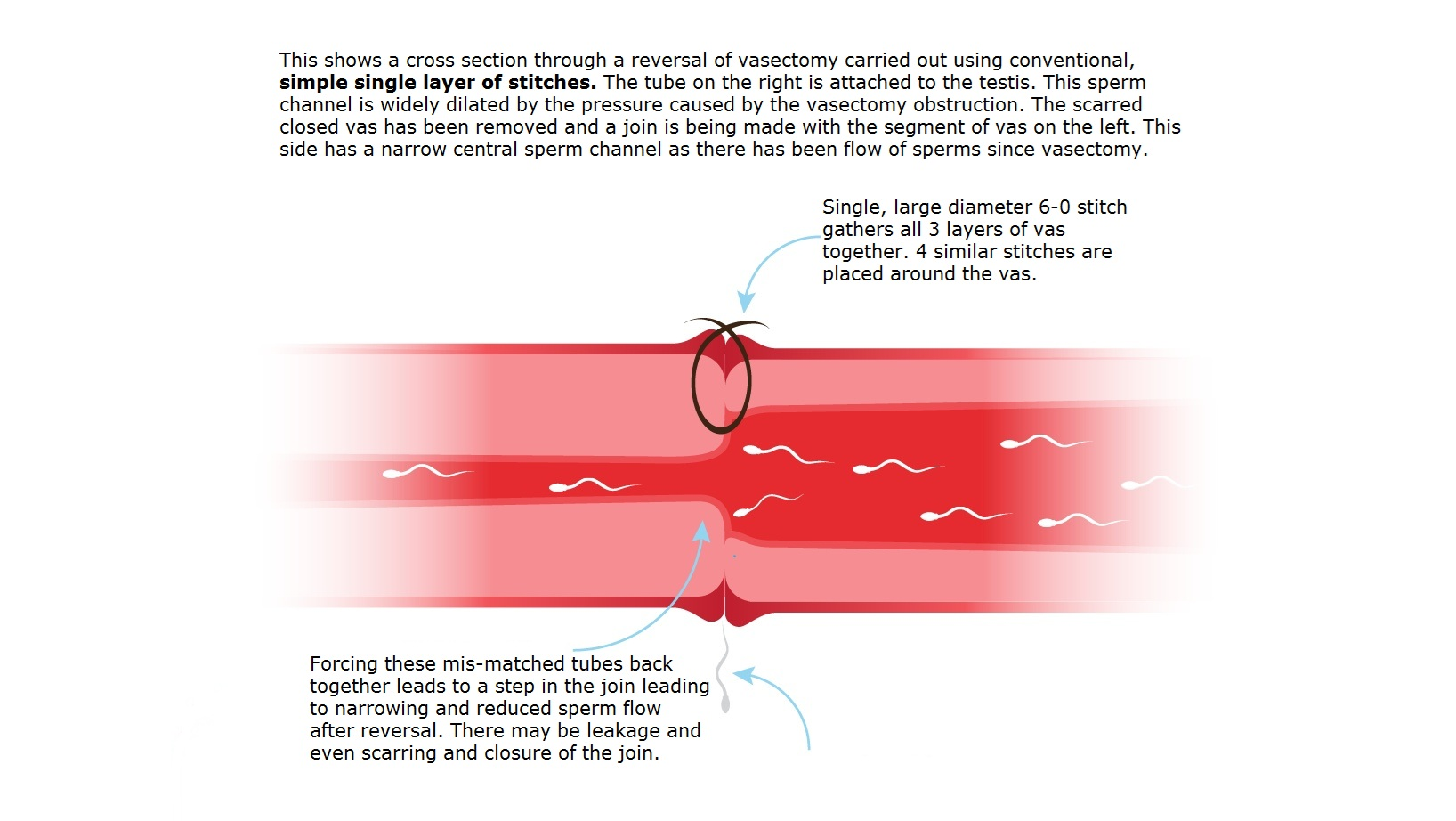
3. The simple method of reconnecting the tube is stitch together the ends using a stitch that goes all the way through all 3 layers of the vas. This brings together the very narrow end of the body side of the vas with the dilated testicle end of the vas leaving a shelf where the two meet as shown in the diagram. The technique is quick for the surgeon who can often manage 6 or 8 operations per day.
4. The consequences of joining the vas in this way are as shown in this diagram, a narrow channel is formed for the sperms to swim through under pressure leading to low sperm counts, poor sperm quality (because they expend too much energy swimming through a narrow junction) and early scarring and closure of the join. This technique is used all across the UK and in clinics that perform reversals quickly with up to 6-8 patients in one day.
5.The Multi layer microdot reversal (MMMV) was developed by professor Goldstein in New York’s Cornell University to improve the pregnancy rates of reversals and make them as free from scarring as humanly possible. Results from Professor Goldstein’s trial of this method show that he has a 99.7% success rate with this technique and pregnancy rate of well over 50%. Here is how it works. Of course the dimensions of the vas are so small that special instruments have been developed for our use. First microscopic 6 ink dots are placed on the ends of the vas to be joined, each the same distance from the skin of the sperm channel. Next, a single micro stitch a needle on each end is placed through each of the 6 dots and the stitch tied together. This joins together the skin layer of the vas very accurately, opening up the narrow end of the vas and gently narrowing the wide testicular end resulting in a smooth, step-free join that is wide open allowing the maximum number of high quality sperms to pass through. Because there are no rough edges in the join, it is rare for scar tissue and closure to form.
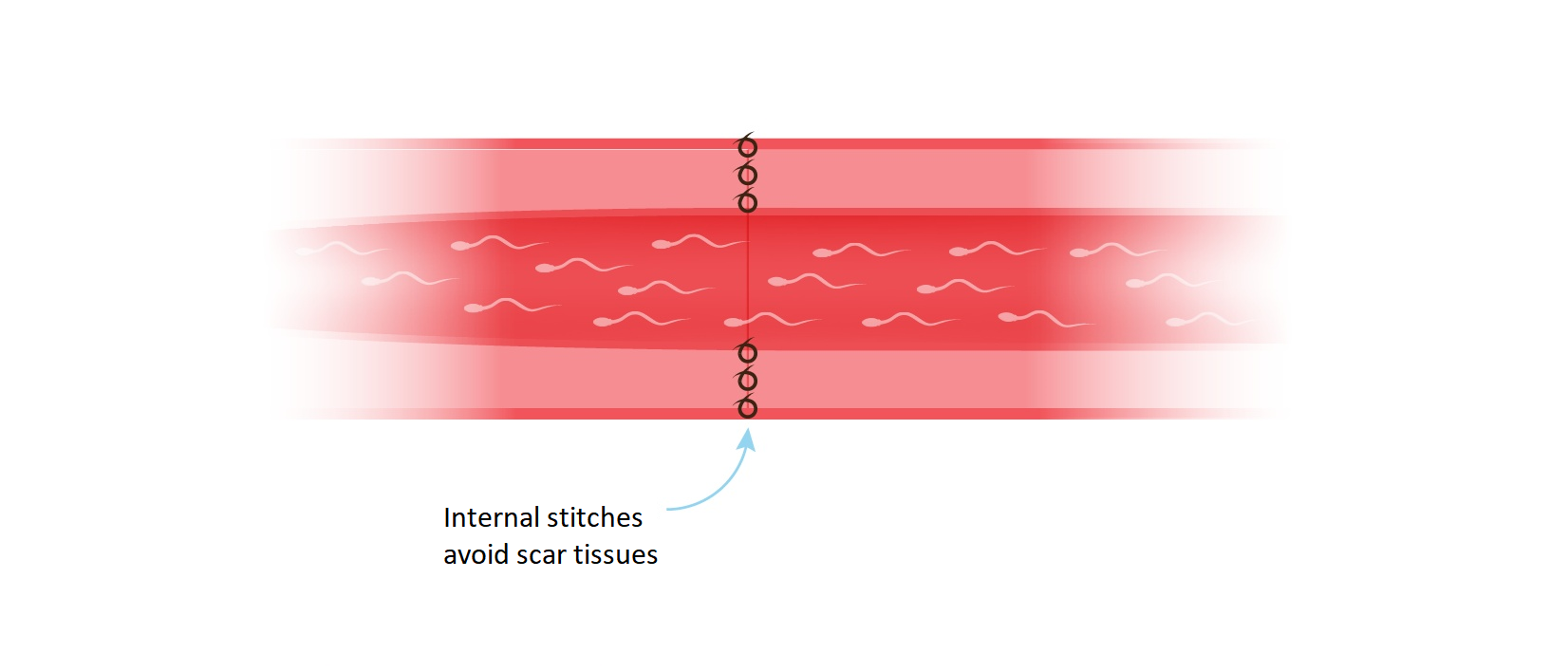
6. The next or second layer of stitches brings the thick muscular layer on the vas together in a leak proof join and finally a third layer of micro stitches joins the outer layers of tissue and blood vessels.
What features make for a successful reversal?
A long distal remnant.
The original vasectomy can be done anywhere between the convoluted vas and the groin ! The longer the tube left on the testicular end of the vas the greater the surface of tube there is to disperse the pressure build up following vasectomy which in turn lessens the chances of a ‘blow out’ blockage in the epididymis.
Sperm granuloma.
This is swelling the size of a small pea on the top end of the distal vas. A granuloma acts as a pressure release valve and reduces the chances of blockage in the epididymis.
Recent vasectomy.
Reversals up to ten years after vasectomy carry a high success rate but after this time there is a steady decline although there are known success even after 20 years !! Microsurgery. This means the placing of the stitches used to repair the tube very accurately with the aid of a microscope. The inner tube of the vas (lumen) measures only 0.2 mm so ultra fine stitches (9.0 and 10.0 – as fine as a human hair) are needed to repair the tube without obstructing it.
Practical Aspects of the Operation
Operation
Lasts approx. 1½ to 2 hours each side.
- Usual Approach via single horizontal or vertical incision
- We locate the vas and the site where the original vasectomy blocked the tube.
- Then we section the tube above and below this area to locate fresh open vas. At this stage we check that the reproductive tract is still functioning by flushing the upper vas with saline and sampling fluid from the testicular vas under the microscope.
- Vasovasostomy ie. joining the ends of vas together using special very fine stitches thinner than a human eyelash (10.0 double armed Nylon sutures specially made in the USA). The medical description of our operation is ‘Multi-layer, microdot microsurgical vasocasostomy’. In this exquisite procedure devised by professor Goldstein, the inner tube of the vas that carries the sperms is microsurgically stitched together followed by the muscle of the wall of the vas. Then the overlying tissue is closed over the top of the repair for strength and to ensure blood supply.
- In selected cases where there is definite signs of blow out, we perform Vaso -epididymostomy at least on one side. This is even more time consuming and delicate procedure
Afterwards.
There are one of two scars approx. 3 cm long – one on each side of the scrotum. We usually close these with a dissolving stitch buried under the skin so that there is no need for further visits to the Clinic. After taking tea and biscuits the patient is accompanied home to rest.
On the night of operation
We recommend that if you live further than an hour’s drive away then you stay the night in a local hotel. We can recommend the local hotels which are relatively less expensive.
Return to work.
The reversals are performed at the beginning of the week will need to rest until Saturday then mobilisation over the weekend and back to work the following Monday just five to seven days after operation.
How will I know if the operation was successful?
We recommend an initial semen test for 12 weeks post-operatively by which time we would expect a return of small numbers of sperm to the semen. Return to full fertility can take 6-8 months so we ask your local GP to arrange for further tests at a pathology lab near you.
What are my chances of becoming fertile again?
This depends on many factors but chiefly the length of time since your vasectomy was performed. This is because the likelihood of the tubes being blocked increases with each year that goes by, however, the operation is successful in more than 80 % of men who had the reversal within up to 10 years after vasectomy. Even if the vasectomy was done more than 10 years ago there is still a worthwhile chance of success
